PGY-1
The clinical rotations and course curriculum in the PGY-1 year foster the resident’s developing identity as a competent and caring physician, through rotations in medicine, neurology, and psychiatry that offer broad clinical experience, excellent teaching, and appropriate levels of responsibility. In addition, residents begin to develop knowledge and skills in the diagnosis, management, and treatment of severely disturbed and mentally ill inpatients. The PGY-1 year is divided into six months of medicine and neurology, four months of adult inpatient psychiatry, and two months of consult/liaison psychiatry. PGY-1s take call at the University of Chicago while on psychiatry, covering the emergency department and the general hospital for psychiatric emergencies, and providing phone consultation for emergent care issues arising on the University of Chicago inpatient psychiatry service at UChicago Medicine Ingalls Memorial. All PGY-1s begin the year with direct supervision from senior residents and progress to greater degrees of independence with attending backup always available.
Primary Care and Neurology: All residents spend two months on the inpatient general medicine service. Additionally, most residents select one month on the general medicine consultation service and one month in the adult emergency department at the University of Chicago. Residents spend two months on the neurology services at the University of Chicago. Those residents who have a particular interest in child psychiatry may choose to spend up to two months on pediatrics (one month inpatient, one month Peds ED), and/or one month on the child neurology service at the University of Chicago Comer Children’s Hospital.
Northshore University Hospital, Adult Inpatient Psychiatry: Two months each during PGY-1 and PGY-2 year are spent on the adult inpatient psychiatric service. Located in Evanston, Northshore is a large and outstanding community hospital with strong ties to the University of Chicago. The patient population is economically and diagnostically varied and includes some patients receiving electroconvulsive therapy (ECT).
UChicago Medicine Ingalls Memorial, Inpatient Psychiatry: Two months each during PGY-1 and PGY-2 year are spent on the adult inpatient psychiatric service. This general psychiatry unit treats acute patients with all major psychiatric disorders, as well as patients with comorbid substance abuse and dependence, and those with some comorbid medical problems. Patients come from the university community including students and staff, from a wide range of communities in the Chicagoland area, and transfers from the University of Chicago emergency department, inpatient medical/surgical, and outpatient psychiatric services.
Consultation/Liaison: Two months each during PGY-1 and PGY-2 year are spent on the CL service at the University of Chicago. The CL service provides psychiatric consultation upon request to hospitalized, adult, medically ill patients. In addition to general consultation, specialist services exist for oncology, transplantation, and neuropsychiatry. The CL team is comprised of CL attendings, a psychosomatic medicine fellow, psychiatry residents, psychology interns, medical students and senior neurology residents and anesthesia pain fellows on a rotating basis. CL residents gain experience in evaluating and managing highly complex medical and surgical patients in a well-supervised teaching service, coupled with the opportunity to participate actively in a multidisciplinary team. To provide a forum for trainees to present and discuss CL and ER cases, a weekly, joint adult and child psychiatry case conference is held. This provides a forum for detailed case discussion and for the presentation of special topics (e.g The Business of CL, Psychotropic Prescribing in Pregnancy, Autoimmune Neuropsychiatric Syndromes).
PGY-2
The PGY-2 year builds on the PGY-1 experiences in medicine and psychiatry, exposing residents to inpatient and outpatient psychiatric treatment in academic, public and private settings with more complex, dually diagnosed and medically comorbid patients. Residents spend two months each on inpatient psychiatry at Ingalls Hospital, inpatient psychiatry at Northshore University, and on the CL service at the University of Chicago. Residents also spend two months on each of the following services: University of Chicago Emergency Psychiatric Service, Chemical Dependency at UChicago Medicine Ingalls Memorial, and Community Psychiatry, an outpatient rotation at Thresholds. PGY-2 residents develop skills as psychiatric educators through increased responsibility for the teaching and supervision of medical students, and through coursework and supervision on education and educational techniques. Residents take call at the University of Chicago with faculty backup by phone.
Chemical Dependency: Residents spend two months on the Chemical Dependency service at UChicago Medicine Ingalls Memorial, under the direction of Dr. Martin Paisner, where patients are admitted for detoxification from a variety of substances of abuse. Residents participate in groups and individual treatment for addictions, attend sobriety maintenance meetings, become familiar with detoxification protocols, and management of patients with dual diagnoses.
Community Psychiatry: Residents spend two months at Thresholds, one of the nation's largest non-profit providers of mental health services. Thresholds offer case management, education, job training and placement, housing, and operates Assertive Community Treatment (ACT) teams providing services to people with serious and persistent mental illness. Residents evaluate new patients and function as part of a team, providing outreach to people in the community in their homes and on the streets as well as in clinics. One day a week is spent at the community psychiatry clinic at Northshore University.
Emergency Psychiatry: Residents spend two months on our Emergency Psychiatry service under the direction of Drs. Marie Tobin and Holly Shiao. Residents provide consultation to the emergency department for management and recommendations on disposition for psychiatric emergencies.
Outpatients: Residents are expected to treat two to three outpatients per week during the PGY-2 year in weekly psychotherapy. Patients are referred from the University of Chicago student health service, as well as the outpatient clinics and inpatient units at the University of Chicago and UChicago Medicine Ingalls Memorial. Residents have two hours of individual supervision, provided by faculty within the Department and the Student Counseling Center (SCS) on campus. Residents also rotate through the Continuing Care (Psychosis) Clinic at the University of Chicago which provides diagnostic evaluations and ongoing medication management for patients with severe and persistent mental illness. Many patients also have serious economic and social problems and major needs for rehabilitation services. This clinic works collaboratively with Thresholds and other community resources to support patients' independence. Several research projects are incorporated into the clinic on the nature and treatment of psychotic disorders.
PGY-3
The PGY-3 year is exclusively an outpatient year. Designed to enable residents to function more independently and to follow a large number of patients longitudinally, PGY-3 provides year-long experience in the general psychiatry clinics, several half-day sessions set aside to see psychotherapy patients, and six-month rotations in subspecialty clinics. Subspecialty clinics include neuropsychiatry, geriatrics, child psychiatry, addictions, anxiety disorders, personality disorders, refractory affective disorders, and several medical/psychiatric clinics including a transplant clinic and a psycho-oncology clinic. Residents provide teaching and supervision for medical students and can participate in internal moonlighting call including providing back-up for PGY-1 residents.
The General Clinics: Adult patients are referred to our clinics from within the University of Chicago system, from inpatient stays on our inpatient psychiatry service, from the surrounding community of Hyde Park where students and faculty live, from the population of hospital and university employees, and from the South Side of Chicago and the greater Northwest Indiana area. Problems vary from complex diagnostic issues to more common affective, anxiety and adjustment disorders. Residents are assigned to one general clinic per week, performing intakes and providing psychiatric follow-up. The clinics are designed to enable residents to pick up a large caseload of patients with varied diagnoses and treatments. Residents have ample opportunity to work collaboratively with psychologists in coordinated treatment. Faculty include Drs. Deborah Spitz and Shoaib Memon.
Specialty Clinics: Residents rotate for six months in a variety of specialty clinics:
- Child Psychiatry—directed by Drs. Khalid Afzal, Seeba Anam, and Stephanie Lichtor, residents provide diagnostic assessment and treatment for children and adolescents with pervasive developmental disorders, disorders of attention, affective disorders, anxiety disorders, psychosis, and eating disorders.
- Geriatrics—directed by Dr. Erin Zahradnik, residents evaluate and manage disorders of mood, cognition, and psychosis in the geriatric population at University of Chicago and at the University of Chicago's South Shore Clinic, which offers integrated geriatric medical and psychiatric care.
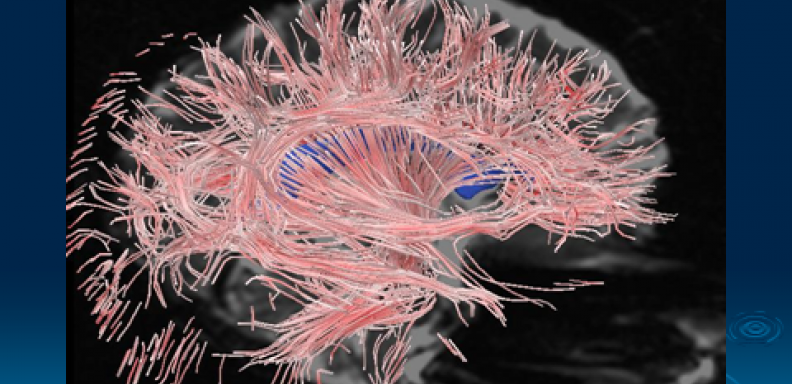
- Neuropsychiatry—this clinic treats patients with complex neuropsychiatric problems including movement disorders, neurodegenerative disorders, epilepsy, MS, traumatic brain injury as well as conversion disorders.
- Anxiety Disorders—directed by Dr. Emil Coccaro and staffed by a psychologist and psychology trainees as well as by residents, this clinic serves patients with severe anxiety disorders, obsessional disorders, panic disorders, and other comorbid psychiatric problems. It offers comprehensive evaluating, pharmacologic treatment, and CBT.
- Medical/Psychiatry—directed by Drs. Marie Tobin, Holly Shiao, Zehra Aftab, and Michael Marcangelo, who attend on the psychiatric consultation/liaison service at the University of Chicago, these clinics offer evaluation and follow-up to patients seen on the C/L service and other patients with comorbid medical and psychiatric problems. Specialized clinics include Transplant with Dr. Aftab and Psycho-oncology with Drs. Tobin and Shiao.
- Personality Disorders—directed by Dr. Royce Lee, this clinic offers assessment and treatment to complex patients with personality disorders and often comorbid affective disorders.
- Refractory Affective Disorders—directed by Dr. Elliot Gershon, this clinic offers highly specialized treatment for patients with severe and refractory unipolar and bipolar disorders. It offers residents the opportunity to use sophisticated psychopharmacologic interventions and gain an understanding of the long-term evolution of severe affective illness.
- Student Counseling Center (SCS)—under the direction of Dr. Erin Hurst, SCS provides emergency consultation, psychoeducation, psychotherapy, and medication management for undergraduate and graduate students at the University of Chicago.
- Women's Mental Health--directed by Zehra Aftab, MD, this clinic evaluates and treats women during pregnancy and the postpartum period as well as women with psychiatric disorders that intersect with reproductive issues.
Outpatients: In addition to patients followed within the general and subspecialty clinics, residents are expected to follow eight hours of outpatients in various modalities of psychotherapy, including psychodynamic psychotherapy, supportive psychotherapy, CBT, combined pharmacologic and psychological treatment, and family therapy. Residents are expected to lead or co-lead at least one group, which may be time-limited and focused on a particular diagnostic issue or problem, or open-ended. Residents receive two and a half hours per week of individual supervision, and additional supervision is available for family and marital cases as well as individual cases for those who request it.
PGY-4
In the PGY-4 year, residents solidify administrative and leadership skills, enlarge clinical confidence and autonomy and focus on individual specialized areas of interest. Each resident assumes a Chief Resident position with significant administrative, supervision and teaching components. Each resident completes a research project and makes a presentation to the Department. Residents continue to follow outpatients in a variety of psychotherapeutic modalities and may choose elective clinical experiences in specialized psychotherapies, such as group or family therapy, psychodynamic psychotherapy, or dialectical behavior therapy, to name a few. All residents gain experience on our Electroconvulsive Therapy service. In conjunction with faculty advisors, each resident develops an individualized schedule for the fourth year that reflects the serious pursuit of particular interests. Some residents choose to focus on research, some emphasize clinical experiences, others assume increased teaching responsibility. The year is designed to allow maximum flexibility so that each resident may pursue a meaningful area in depth.
Chief Residencies: Two PGY-4s serve as Administrative Chief residents, leading Residents Meeting and working closely with the Residency Training Directors on administrative issues. Chief residents on the inpatient units, the consultation/liaison service, outpatient clinics, and the emergency service at the University of Chicago provide administrative leadership, teaching and supervision for medical students and junior residents on those services, leading case conferences and designing and teaching specialized courses. There is flexibility in each of these roles, and specific duties may be negotiated with the Program Director, based on the resident’s interests; for example, one fourth-year resident devised a chief residency in Medical Student Education, helping to redesign the psychiatry clerkship and focus on recruitment of medical students into psychiatry.
Research: Under the supervision of faculty research mentors and with the guidance of the Research Seminar led by Dr. Kristen Jacobsen, each resident completes a research project in collaboration with one of several research groups in the Department. The resident presents the research to the Department in June of the PGY-4 year. Some residents choose to spend a large portion of the PGY-4 year on larger research projects, and many have published their work and/or presented at national meetings.
Forensic Psychiatry: All residents evaluate and write up a forensic case under the direction of one of the Department’s forensic psychiatrists, Drs. Daniel Yohanna, Jon Grant, Caroline Shima, and Sandy Finkel.
Electroconvulsive Therapy: Residents gain experience in the outpatient evaluation of patients referred for ECT, the indications and relative contraindications for ECT, the informed consent process, the delivery of treatment and ongoing monitoring of psychiatric, cognitive and medical symptoms during acute course and maintenance phases of ECT. For interested residents, an extended elective experience in ECT, leading to eligibility for certification of advanced training in ECT upon graduation, is available.
Elective Clinical Experiences:
Specialty Clinics: Resident can choose to spend six months in any of the above specialty clinics that they didn't experience in PGY-3.
Intensive Sequence Elective: In conjunction with a course which reviews classic psychoanalytic theory under the direction of Dr. Harry Trosman, a senior psychoanalyst, the resident treats 2-3 patients for one year in intensive (two or three times per week) psychotherapy, with supervision provided by psychoanalysts affiliated with the Chicago Institute for Psychoanalysis.
Family Institute Elective: Residents can take courses and evaluate and treat families at the Family Institute in Downtown Chicago.
Women's Mental Health: Residents can elect an outpatient experience and reading course focused on Women's Mental Health.
Other Electives: Clinical, research, and educational electives are arranged individually.